Introduction: Patients with T-cell lymphoma have variable clinical manifestations and outcomes depending on the histology and their response to therapies. However, the overall outcomes are not as good as their B-cell lymphoma counterpart with induction chemotherapy alone. Therefore, autologous transplant is often used as consolidation in first remission or at relapse because of the poor outcomes with conventional therapy. We have reported previously on Stanford experience of these patients who underwent autologous transplant before 2007 (BBMT 2008, 14:741). Here, we reported a retrospective review of patients in the modern era (2008-2018) with emphasis on the impact of pre-transplant disease status on outcomes and post-transplant relapse management.
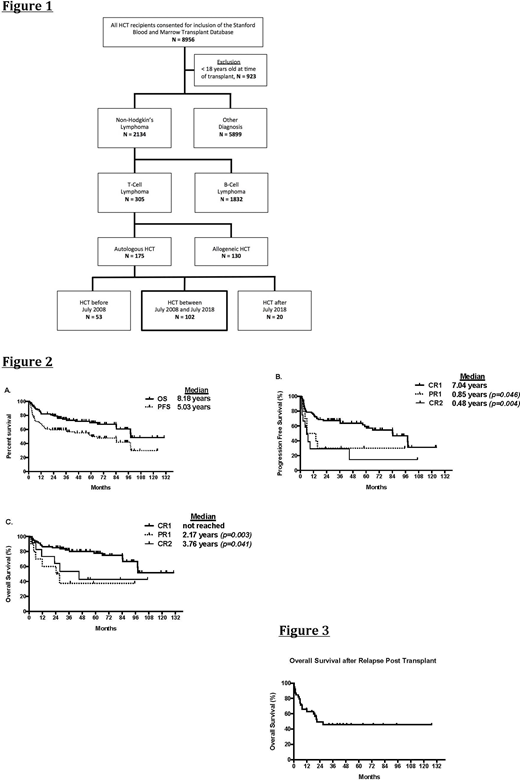
Method: Between July 1, 2008 and July 31, 2018, 102 consecutive patients with T-cell lymphoma received high dose chemotherapy/autologous hematopoietic cell rescue at Stanford and constitute the study cohort (Figure 1). This study cohort was selected for adequate follow-up (>2 years) after transplant. Progression free survival (PFS) and overall survival (OS) was estimated from the date of transplant using the Kaplan-Meier method. PFS and OS were compared between groups with different pre-transplant disease status based on response to the last pre-transplant therapies (CR1 vs. PR1 vs. CR2).
Result: This study cohort included patients with peripheral T-cell lymphoma, non-specified (n=21), angioimmunoblastic T-cell lymphoma (n=50), ALK-negative anaplastic large-cell lymphoma (n=14), ALK-positive anaplastic large-cell lymphoma (n=5), extranodal NK/T cell lymphoma (n=9), enteropathy-type T-cell lymphoma (n=1), adult T-cell leukemia/lymphoma (n=1) and hepatosplenic T-cell lymphoma (n=1). It had a male/female ratio of 61/41, and a median age of 58 years (range 23-71). At diagnosis the majority of the patients had stage III/IV disease (70%) and B symptoms (56%). The median time from diagnosis to transplant was 8.1 months (range 4-176). The majority of patients were in first complete remission (CR1, n=79) at the time of transplant, while others were in PR1 (n=11) or in CR2 (n=12) from last pre-transplant therapies. Ninety-one (89%) patients received high dose cyclophosphamide/carmustine/etoposide(CBV) and 11 patients received high dose carmustine/etoposide/cytarabine/melphalan (BEAM) prior to autograft infusion. Median follow-up post-transplant was 36.8 months (range 0.7-130) for the entire cohort.
The estimated 3-year PFS and OS were 60% (95% CI 49-68%) and 75% (95% CI 65-82%), respectively (Figure 2A). Patients who were in CR1 had significantly better median PFS compared to patients in PR1 or CR2 (7.04 vs 1.19 years, p=0.039; 7.04 vs 0.48 years p=0.004, Figure 2B). The estimated 3-year PFS were 67% (95% CI 55-76%), 36% (95% CI 11-63%), and 29% (95% CI 8-56%) for the CR1, PR1 and CR2 groups respectively. Patients who were in CR1 also had significantly better median OS compared to patients in PR1 or CR2 (not reached vs 2.30 years, p=0.018; not reached vs 3.76 years p=0.045, Figure 2C).The estimated 3-year OS were 82% (95% CI 71-89%), 44% (95% CI 14-70%), and 53% (95% CI 21-78%) for the CR1, PR1 and CR2 groups respectively. In this cohort, there were no significant differences in either PFS or OS between different histology.
Forty patients experienced disease relapse after transplant. The majority (n=28, 70%) of these patients received additional therapies including chemotherapy (n=13), brentuximab vedotin (n=12), HDAC inhibitor (n=7), and radiation (n=3) with a median systemic therapy of 2 (range 1-5). Thirteen patients eventually underwent allogeneic hematopoietic cell transplantation. The median OS after post-transplant relapse was 21.3 months (Figure 3). Both brentuximab vedotin and allogeneic transplant seemed to provide prolonged survival for these relapsed patients, with estimated 2-year post-relapse OS were 75% (95% CI 13-96%) and 63% (95% CI 28-84%) for the two groups respectively.
Conclusion: Autologous transplant remains to be a good option as consolidation for patients with T-cell lymphoma, mostly in patients with first complete remission. While close to 40% of the patients experienced relapse after autologous transplant, additional therapies such as brentuximab vedotin or/and allogeneic transplant can provide long-term benefit for these patients.
Shizuru:Jasper Therapeutics, Inc: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees. Shiraz:Kite, a Gilead Company: Research Funding; ORCA BioSystems: Research Funding. Muffly:Servier: Research Funding; Amgen: Consultancy; Adaptive: Research Funding. Sidana:Janssen: Consultancy. Meyer:Orca Bio: Research Funding. Rezvani:Pharmacyclics: Research Funding. Miklos:Novartis: Consultancy, Other: Travel support, Research Funding; Pharmacyclics: Consultancy, Other: Travel support, Patents & Royalties, Research Funding; Allogene Therapeutics Inc.: Research Funding; Kite-Gilead: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel support, Research Funding; Juno-Celgene-Bristol-Myers Squibb: Consultancy, Other: Travel support, Research Funding; Janssen: Consultancy, Other: Travel support; Miltenyi Biotec: Research Funding; Adaptive Biotech: Consultancy, Other: Travel support, Research Funding. Negrin:Magenta Therapeutics: Consultancy, Current equity holder in publicly-traded company; Biosource: Current equity holder in private company; Amgen: Consultancy; BioEclipse Therapeutics: Current equity holder in private company; UpToDate: Honoraria; KUUR Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal